The plan aims to increase patient conversion rates into the CCM program through strategic metrics and targeted improvements. Each metric is crucial as it highlights areas to enhance, ensuring successful patient transitions. Conversion Rate is pivotal, focusing on the percentage of patients enrolling, with benchmarks like 20-30% guiding strategies. For instance, offering flexible options aids conversion.
Call Volume and Call to Conversion Time are equally essential, emphasizing efficiency and prompt patient handling. With benchmarks set at 1000 calls per week and 1-2 weeks for conversion, these metrics indicate the need for streamlined processes and proactive communication. Additionally, a high Patient Satisfaction Score of 80% reflects the quality of interactions, crucial for long-term retention.
Top 5 metrics for Increase patient conversion rate
1. Conversion Rate
The percentage of patients called who enroll in the CCM program
What good looks like for this metric: 20-30%
How to improve this metric:- Provide detailed information about CCM benefits
- Offer flexible enrollment options
- Follow up with hesitant patients
- Highlight positive testimonials
- Simplify the enrollment process
2. Call Volume
The total number of calls made to potential CCM patients
What good looks like for this metric: 1000 calls per week
How to improve this metric:- Increase the size of the call team
- Use automated dialers
- Extend calling hours
- Prioritise high-potential leads
- Track call completion rates
3. Call to Conversion Time
The average time taken from the first call to patient enrollment in the program
What good looks like for this metric: 1-2 weeks
How to improve this metric:- Streamline follow-up processes
- Clarify onboarding steps during calls
- Offer quick response channels
- Maintain communication through multiple formats
- Address patient queries swiftly
4. Patient Satisfaction Score
Patient-reported happiness with the call and enrollment process
What good looks like for this metric: 80% satisfaction
How to improve this metric:- Conduct surveys post-enrollment
- Gather feedback on call quality
- Enhance training for callers
- Resolve queries efficiently
- Personalise communication
5. Retention after Enrollment
The percentage of patients remaining in the CCM program after a set period
What good looks like for this metric: 60-70% after 6 months
How to improve this metric:- Implement engagement strategies
- Monitor patient progress regularly
- Provide value-added services
- Build strong relationships
- Continually assess patient needs
How to track Increase patient conversion rate metrics
It's one thing to have a plan, it's another to stick to it. We hope that the examples above will help you get started with your own strategy, but we also know that it's easy to get lost in the day-to-day effort.
That's why we built Tability: to help you track your progress, keep your team aligned, and make sure you're always moving in the right direction.
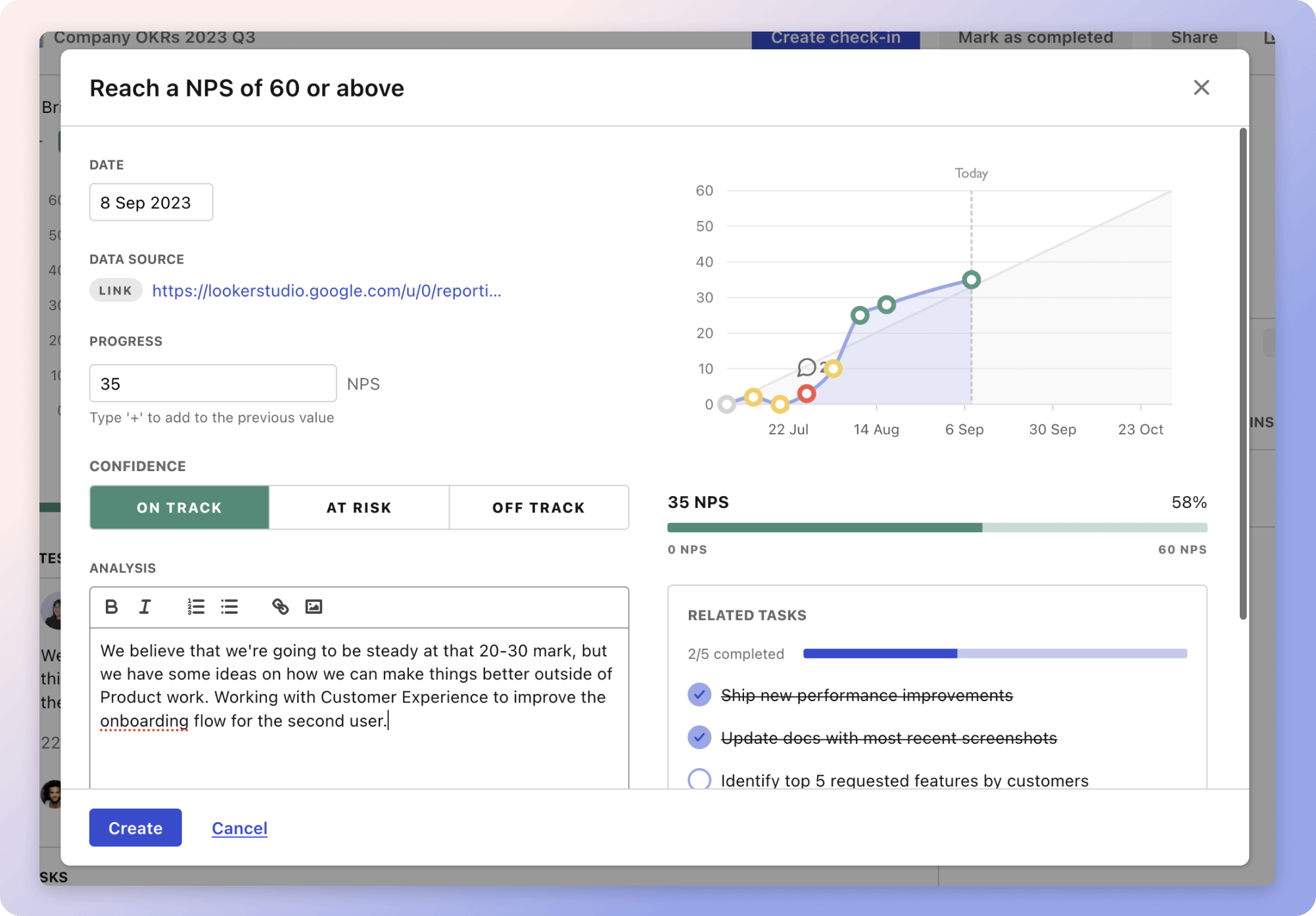
Give it a try and see how it can help you bring accountability to your metrics.